Night Terrors in Children
Night Terrors in Children
Night terrors are a common sleep disorder that can affect children, causing them to experience intense fear and confusion during their sleep. As a parent or caregiver, it can be distressing to witness your child going through night terrors.
What are Night Terrors?
Night terrors, also known as sleep terrors, are episodes of intense fear or terror that occur during sleep. They usually occur within few hours after bedtime. Unlike nightmares, after a night terror a child is not able to remember the dream when he or she awakens in the morning.
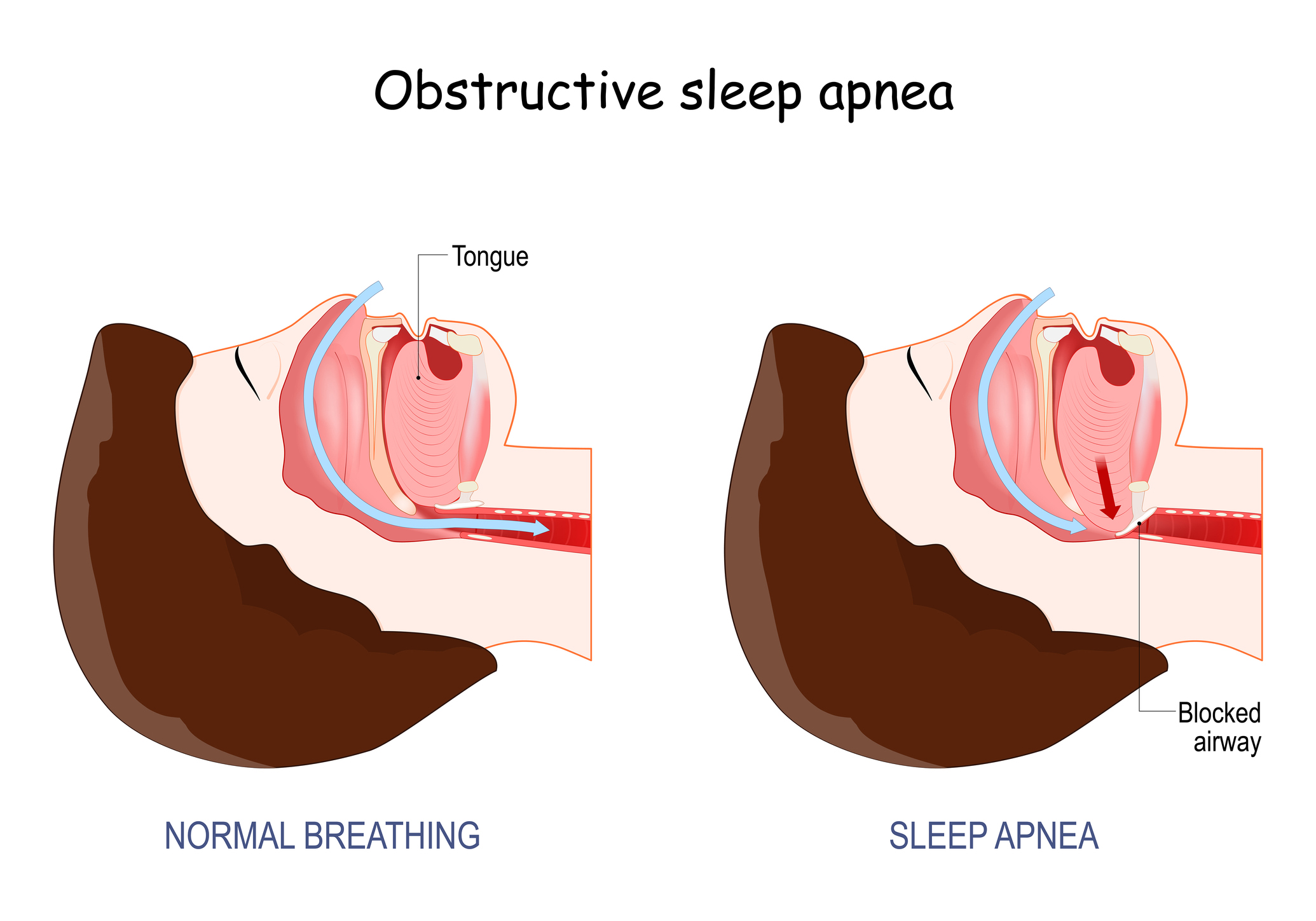
Night terrors are more common in children aged 3 to 8 years but can occur at any age. Sometimes, recurring sleep terrors are a symptom of other sleep disorders like obstructive sleep apnea. They affect 2% to 7%of children and usually peak between ages 4 and 7. Most children outgrow them before their teens.
Causes:
The exact causes of night terrors are not fully understood, but several factors can contribute to their occurrence including:
- Overstimulation: Overtiredness, exhaustion, or disrupted sleep patterns can trigger night terrors.
- Genetics: A family history of night terrors or other sleep disorders may increase the likelihood of a child experiencing them.
- Stress or Anxiety: Emotional stress, anxiety, or significant life changes can contribute to night terrors in some children.
- Fever or Illness: High fevers or certain illnesses may be associated with an increased risk of night terrors.
- Obstructive Sleep Apnea (OSA) –untreated OSA increases the amount of arousals children have overnight and can increase the risk of night terrors occurring, This should particularly be considered if they are having multiple night terrors a week or in the same night as that would be an abnormal frequency for night terrors alone.
Symptoms:
Recognizing the signs of night terrors can help you differentiate them from other sleep disturbances. Common symptoms include:
- Sudden awakening from sleep with a look of intense fear
- Loud screaming or crying that is difficult to console
- Rapid breathing and increased heart rate
- Sweating and physical agitation
- Difficulty recognizing or interacting with others during the episode
- Limited or no memory of the even upon awakening
Managing Your Child’s Night Terrors:
While they can be distressing, there are several steps you can employ to help your child through a night terror
- Maintain a Consistent Sleep Schedule: Establish a regular sleep routine to ensure your child gets enough restful sleep each night. Consistency can help prevent overstimulation and reduce the occurrence of night terrors.
- Create a Soothing Bedtime Routine: Implement calming activities before bedtime, such as reading a book or taking a warm bath. This can help your child relax and transition into sleep more easily.
- Create a Safe Sleep Environment: Make sure your child’s bedroom is safe and free from any potential hazards. Use a night light if your child feels more comfortable with some light in the room.
- Minimize Stress and Anxiety: Encourage open communication with your child and provide reassurance and support during the day. If your child is experiencing stress or anxiety, consider incorporating relaxation techniques, such as deep breathing exercises or visualization, into their daily routine.
- Avoid Triggers: Identify and minimize potential triggers for night terrors, such as certain foods, drinks, or activities close to bedtime. Additionally, limit exposure to stimulating media before sleep.
- Ensure Safety During Episodes: If your child experiences a night terror, make sure they are safe by gently guiding them back to bed without waking them fully. Attempting to wake or restrain them may prolong the episode or increase distress.
- Seek Professional Advice: If night terrors persist or significantly affect your child’s well-being or daily functioning, consider consulting your pediatrician or a sleep medicine professional for further evaluation and guidance.
Night terrors can be unsettling for both children and parents, but with understanding and effective strategies, they can be managed. By creating a consistent sleep routine, providing a supportive environment, and minimizing potential triggers, you can help your child navigate through night terrors and ensure they have a restful night’s sleep.
Our sleep medicine specialists at Comprehensive Sleep Care Center can determine whether these events are night terrors or whether they are symptoms of a more serious sleep disorder like sleep apnea. Our doctors will combine the information they learn from your child’s sleep history, physical exam, and other test, like a sleep study, to make the diagnosis.