Sleep Awareness Week 2025: Why Quality Sleep Matters and How We Can Help
Sleep Awareness Week 2025: Why Quality Sleep Matters and How We Can Help
March 10-16 marks the 27th annual Sleep Awareness Week, a national campaign dedicated to highlighting the importance of sleep and how it impacts overall health and well-being. Quality sleep is essential for physical, mental, and emotional health, yet millions of Americans struggle with sleep-related issues. At Comprehensive Sleep Care Center, we are committed to helping you achieve the restful sleep you need to live a healthier, more fulfilling life.
The Importance of Quality Sleep
Sleep is more than just a nightly routine—it is a pillar of good health, just as important as diet and exercise. Here’s how getting quality sleep benefits you:
- Boosts Immune Function: Your body repairs and regenerates during sleep, strengthening your immune system and helping you fight off illness.
- Enhances Brain Function: Sleep improves memory, cognitive function, and problem-solving skills, making you more productive and alert.
- Supports Heart Health: Poor sleep is linked to high blood pressure, heart disease, and an increased risk of stroke.
- Regulates Mood and Mental Health: Lack of sleep can contribute to stress, anxiety, and depression, while quality sleep helps balance emotions and improve overall well-being.
- Aids in Weight Management: Sleep plays a crucial role in regulating hunger hormones, helping you maintain a healthy weight.
Signs You May Have a Sleep Disorder
If you experience any of the following symptoms, it may be time to seek professional help:
- Constant fatigue despite a full night’s sleep
- Difficulty falling or staying asleep
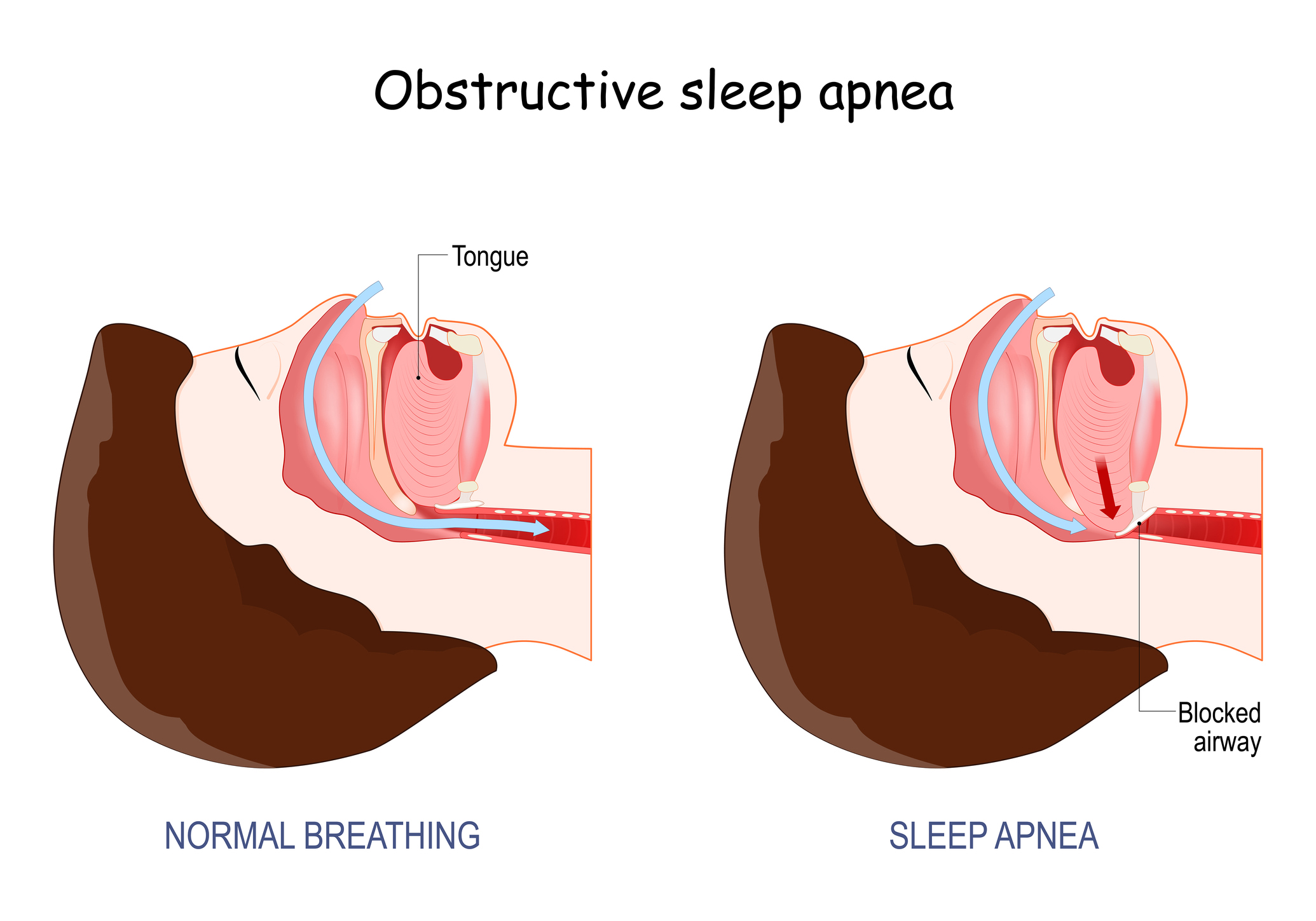
- Frequent snoring or gasping for air during sleep
- Morning headaches or dry mouth
- Difficulty concentrating or mood swings
How Comprehensive Sleep Care Center Can Help
At Comprehensive Sleep Care Center, we specialize in diagnosing and treating a wide range of sleep disorders, including sleep apnea, insomnia, restless legs syndrome, narcolepsy, and more. Our team of sleep experts offers:
- State-of-the-Art Sleep Studies: Our advanced in-lab and at-home sleep testing options provide precise diagnoses.
- Customized Treatment Plans: From CPAP therapy and oral appliances to behavioral therapy, we tailor treatments to fit your unique needs.
- Expert Medical Team: Our board-certified sleep physicians, physician assistants, and sleep specialists are dedicated to helping you sleep better.
- Convenient Locations: We have multiple locations to make expert sleep care easily accessible.
Prioritize Your Sleep Today
This Sleep Awareness Week, make a commitment to prioritize your sleep. If you or a loved one are struggling with sleep issues, don’t wait—Comprehensive Sleep Care Center is here to help. Contact us today to schedule a consultation and take the first step toward a healthier, well-rested life.
Sleep better. Live better.