Sleep Apnea and Heart Disease: What You Need to Know
Sleep Apnea and Heart Disease: What You Need to Know
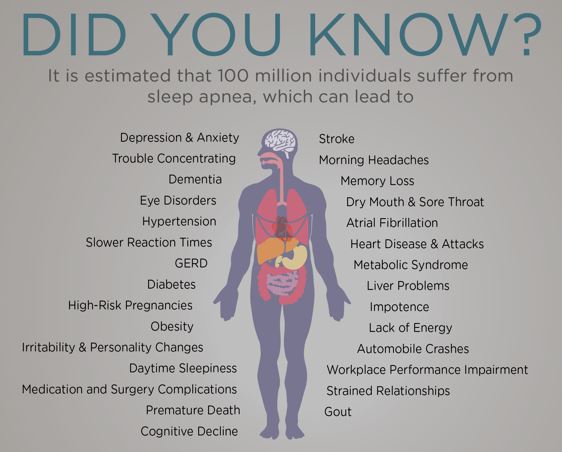
Heart Health Month is the perfect time to talk about an often-overlooked connection: sleep apnea and cardiovascular disease. Many people know that sleep is important for overall wellness, but fewer realize just how strongly untreated sleep apnea can impact heart health.
At Comprehensive Sleep Care Center, we help patients understand these risks and provide expert diagnosis and treatment to protect both sleep and heart health.
What Is Sleep Apnea?
Sleep apnea is a serious sleep disorder in which breathing repeatedly stops and starts during sleep. These pauses in breathing reduce oxygen levels and force the body to work harder throughout the night. Over time, this stress can significantly affect the heart and blood vessels.
The most common type is obstructive sleep apnea (OSA), caused by airway collapse during sleep. Many people with sleep apnea are unaware they have it.
Common symptoms include:
- Loud snoring
- Gasping or choking during sleep
- Excessive daytime sleepiness
- Morning headaches
- Difficulty concentrating
How Sleep Apnea Affects Heart Health
Untreated sleep apnea places repeated strain on the cardiovascular system. Each breathing pause triggers a surge in stress hormones, increases blood pressure, and lowers oxygen levels — all of which raise the risk of serious heart conditions.
High Blood Pressure (Hypertension)
Sleep apnea is a leading cause of secondary hypertension. The repeated drops in oxygen during sleep cause blood pressure to rise and remain elevated, even during the day. Patients with sleep apnea often struggle with blood pressure that is difficult to control despite medication.
Treating sleep apnea can significantly improve blood pressure control and reduce long-term cardiovascular risk.
Stroke Risk
Sleep apnea is strongly linked to an increased risk of stroke. Poor oxygen delivery to the brain, combined with high blood pressure and inflammation, can damage blood vessels over time. Studies show that untreated sleep apnea increases both the likelihood of having a stroke and the risk of poor recovery afterward.
Early diagnosis and treatment can help lower this risk and support better brain and vascular health.
Atrial Fibrillation (AFib)
Atrial fibrillation (AFib) is a common heart rhythm disorder that can lead to blood clots, stroke, and heart failure. Sleep apnea increases the risk of developing AFib and makes it more difficult to manage.
Patients with untreated sleep apnea are more likely to experience:
- Recurring AFib episodes
- Poor response to medications
- Higher rates of AFib recurrence after procedures
Treating sleep apnea can improve AFib outcomes and reduce cardiovascular complications.
Why Sleep Apnea Often Goes Undiagnosed
Many patients assume snoring or fatigue is normal, while others may not connect sleep problems with heart symptoms. Because sleep apnea develops gradually, it often goes undetected for years — allowing cardiovascular damage to progress silently.
If you have heart disease, high blood pressure, a history of stroke, or AFib, a sleep evaluation is especially important.
Diagnosing Sleep Apnea at Comprehensive Sleep Care Center
At Comprehensive Sleep Care Center, we offer comprehensive sleep apnea testing options, including:
- In-lab sleep studies
- At-home sleep apnea testing (when appropriate)
Our board-certified sleep specialists carefully evaluate each patient to determine the most accurate diagnosis and personalized treatment plan.
Sleep Apnea Treatment Options
Effective treatment of sleep apnea not only improves sleep quality — it can also significantly reduce cardiovascular risks.
Common treatment options include:
Positive Airway Pressure (PAP) Therapy
PAP therapy remains the gold standard for treating moderate to severe sleep apnea. It keeps the airway open throughout the night, improving oxygen levels and reducing strain on the heart.
Oral Appliance Therapy
For some patients with mild to moderate sleep apnea, custom oral appliances can help reposition the jaw to keep the airway open.
Lifestyle and Medical Management
Weight management, positional therapy, and addressing nasal or airway issues may also play a role in treatment.
Our team works closely with patients and referring cardiologists to ensure coordinated care.
Protect Your Heart by Prioritizing Sleep
This Heart Health Month, take a closer look at how well you’re sleeping. If you or a loved one has symptoms of sleep apnea — especially alongside heart disease, high blood pressure, stroke, or AFib — evaluation and treatment could be life-changing.
Better sleep supports a healthier heart.
Schedule a Sleep Evaluation
If you’re concerned about sleep apnea and heart health, contact Comprehensive Sleep Care Center today to schedule a consultation with our experienced sleep specialists.
Comprehensive Sleep Care Center is proud to serve patients at the following locations: