Sleep Divorce: The Importance of Treating Sleep Apnea for a Harmonious Bedroom
Sleep Divorce: The Importance of Treating Sleep Apnea for a Harmonious Bedroom
Sleep is an essential part of our lives, and for many couples, sharing a bed can be a beautiful way to connect and bond. However, what happens when snoring becomes a disruptive force, leading to a phenomenon known as a “sleep divorce”? In this blog, we’ll explore the concept of a sleep divorce, its impact on relationships, and why it’s crucial to get tested and treated for sleep apnea to get back in the bedroom and rekindle the romance.
The Sleep Divorce: An Unwanted Separation
A sleep divorce is not a legal separation but rather a scenario where one partner, often due to snoring, is forced to leave the bedroom and sleep in another room. While it may seem like a harmless solution to get a good night’s sleep, it can have profound effects on the relationship. Sleeping separately can lead to feelings of isolation, disconnection, and even intimacy issues, which, if left unaddressed, can harm the partnership.
The Role of Sleep Apnea
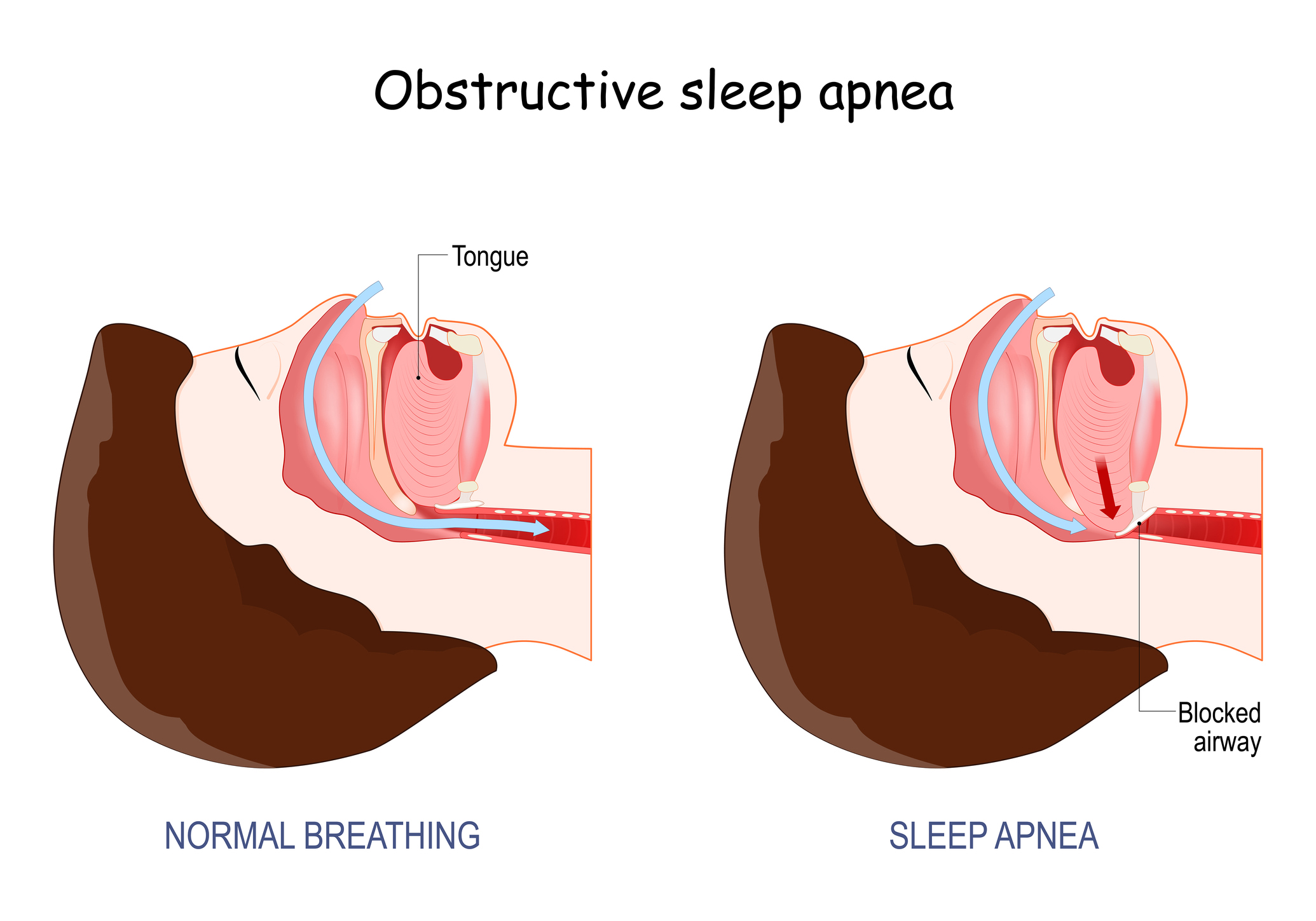
One of the most common reasons for disruptive snoring and the need for a sleep divorce is obstructive sleep apnea (OSA). Sleep apnea is a serious sleep disorder in which breathing repeatedly stops and starts during sleep. This condition not only affects the quality of sleep but also puts the affected individual at risk for various health issues, including heart disease, stroke, and diabetes.
When one partner has sleep apnea, the other may suffer from sleep deprivation due to the loud snoring and frequent awakenings. This sleep deprivation can lead to frustration and ultimately drive a wedge between partners. However, what many couples don’t realize is that sleep apnea is a treatable condition.
The Importance of Testing and Treatment
If you or your partner is experiencing the symptoms of sleep apnea, such as loud snoring, choking or gasping during sleep, and excessive daytime sleepiness, it’s crucial to seek professional help. A sleep study, conducted either in a sleep clinic or at home, can diagnose sleep apnea and determine its severity.
Once diagnosed, effective treatment options are available, including:
- Continuous Positive Airway Pressure (CPAP) Therapy: This involves wearing a mask that delivers a continuous flow of air to keep the airways open during sleep.
- Oral Appliance Therapy: Custom-made oral devices can help reposition the jaw and tongue to prevent airway blockage.
- Lifestyle Modifications: Weight loss, avoiding alcohol and sedatives, and changing sleep positions can sometimes alleviate mild sleep apnea.
- Surgical Interventions: In severe cases, surgery may be recommended to remove excess tissue or correct structural issues causing airway obstruction.
Getting Back in the Bedroom
By seeking treatment for sleep apnea, you can improve not only your health but also your relationship. When snoring and sleep apnea are under control, partners can return to sharing a bed, fostering a more intimate and connected relationship. A restful night’s sleep benefits both individuals, leading to better physical and emotional well-being.
A sleep divorce caused by snoring and untreated sleep apnea can strain even the strongest relationships. It’s essential to recognize the signs of sleep apnea, seek professional help, and commit to treatment. By doing so, you can eliminate the need for a sleep divorce, rekindle the romance in your relationship, and enjoy the benefits of sharing a bed once again. Remember, a good night’s sleep can lead to happier mornings and a healthier, happier partnership.
If you have sleep related issues contact our sleep medicine providers at Comprehensive Sleep Care Center and Say Hello to Sleep Again…