Better Sleep, Better Health in 2026
Better Sleep, Better Health in 2026
As we welcome 2026, many people focus on resolutions like eating healthier, exercising more, or managing stress. But one of the most powerful—and often overlooked—keys to better health is better sleep.
Quality sleep is not a luxury. It is essential to your physical health, mental well-being, and overall quality of life. At Comprehensive Sleep Care Center, we encourage patients to make sleep a priority in the New Year—for better days and healthier years ahead.
Why Sleep Matters More Than Ever
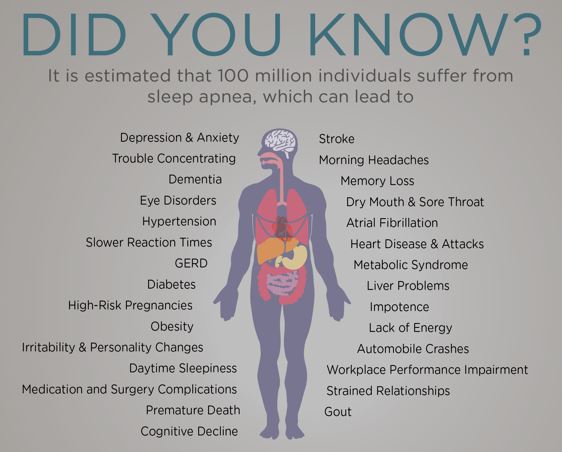
Sleep plays a critical role in nearly every system in your body. When sleep is poor or disrupted, it can increase your risk for:
-
Heart disease and high blood pressure
-
Diabetes and weight gain
-
Memory problems and difficulty concentrating
-
Mood changes, anxiety, and depression
-
Fatigue and reduced daytime performance
If you’re waking up tired, snoring loudly, struggling to stay awake during the day, or feeling unrefreshed even after a full night’s sleep, you may be experiencing an undiagnosed sleep disorder.
Common Sleep Disorders That Affect Your Health
Many people live with sleep disorders without realizing it. Some of the most common include:
Sleep Apnea
A serious condition where breathing repeatedly stops during sleep. Untreated sleep apnea increases the risk of heart attack, stroke, and arrhythmias.
Insomnia
Difficulty falling or staying asleep, leading to chronic fatigue and reduced quality of life.
Restless Legs Syndrome & Other Sleep Disorders
Conditions that disrupt sleep quality and prevent restorative rest.
The good news? These conditions are highly treatable with proper diagnosis and care.
New Year, New Sleep Goals
The start of a new year is the perfect time to focus on improving your sleep habits and addressing ongoing sleep concerns. Simple steps can make a big difference:
-
Stick to a consistent sleep schedule
-
Create a calm, screen-free bedtime routine
-
Avoid caffeine and alcohol close to bedtime
-
Seek professional help if sleep problems persist
If lifestyle changes aren’t enough, a sleep evaluation may be the next step.
How Comprehensive Sleep Care Center Can Help
At Comprehensive Sleep Care Center, we specialize in diagnosing and treating sleep disorders with personalized care. Our services include:
-
In-lab and at-home sleep studies
-
CPAP therapy for sleep apnea
-
Oral Appliance Therapy for patients seeking a CPAP alternative
-
Ongoing support to ensure long-term success and better sleep outcomes
Our experienced team works closely with you to develop a treatment plan that fits your needs, lifestyle, and health goals.
Make Better Sleep Your Resolution for 2026
Better sleep leads to better energy, better focus, better heart health, and better overall wellness. As you plan for a healthier 2026, don’t underestimate the power of a good night’s sleep.
If you or a loved one are experiencing sleep issues, now is the time to take action.
Start the New Year with better sleep—and a healthier you.
👉 Schedule a sleep consultation Here with Comprehensive Sleep Care Center today.
Comprehensive Sleep Care Center is proud to serve patients at the following locations: